The primary care workforce in Massachusetts is under significant strain, with state residents facing challenges in accessing basic preventive care. This growing crisis means patients are often unable to receive timely and essential health services necessary for maintaining overall well-being. In response, the Massachusetts Health Policy Commission (HPC) has proposed a series of forward-looking recommendations aimed at remedying the situation and ensuring better healthcare access. This article explores the common themes, key points, overarching trends, and consensus viewpoints related to the primary care shortage and the actionable proposals put forth by the HPC.
Provider Shortage and Financial Disparities
The Growing Provider Shortage
Massachusetts is experiencing a significant shortage of new providers entering the field of primary care. This shortage is creating a critical gap in basic healthcare services, especially for residents in rural areas with already limited access to medical care. The aging workforce, coupled with an insufficient influx of new graduates into the field, has exacerbated the problem, making it increasingly difficult for residents to receive timely and necessary care. This shortage is not merely a numbers issue; it impacts the overall quality of healthcare and patient outcomes across the state.
The scarcity of primary care providers has far-reaching implications. Healthcare systems and individual providers are stretched thin, leading to longer wait times and reduced availability of services. In rural areas, the deficit is more pronounced, where geographic barriers already pose a challenge to accessing care. Efforts to address this gap must focus on both attracting new providers to the field and retaining those currently practicing. Strategies to bolster the workforce are essential to ensure every Massachusetts resident has access to a primary care provider when they need one.
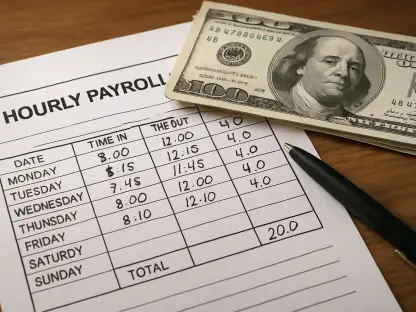
Financial Disparities in Reimbursement Rates
Primary care providers receive lower reimbursement rates compared to their specialist counterparts, which significantly discourages new graduates from entering the field. This financial disparity presents a major deterrent, as medical school graduates are often drawn to specialties that offer higher financial incentives. The HPC report highlights the stark reality that primary care spending has grown only half as fast as spending on all other medical services from 2017 to 2022, indicating a compelling need for financial rebalancing to make primary care more appealing.
Reimbursing primary care providers at higher rates is crucial to leveling the playing field and encouraging more providers to pursue careers in primary care. Lower reimbursement rates not only affect individual provider incomes but also impact the financial viability of primary care practices, especially independent ones and community health centers. The current trend results in fewer medical graduates choosing primary care residencies, further contributing to the workforce shortage. Addressing these financial disparities could help shift this trend, creating a more robust and sustainable primary care workforce in Massachusetts.
Unsustainable Workloads and Burnout
High Workloads Leading to Burnout
Primary care providers in Massachusetts are facing unsustainable workloads, contributing significantly to professional burnout and a reduction in the number of practicing providers. The HPC report identifies administrative tasks such as billing, coding, and prior authorizations as major factors in this burnout. Providers are spending disproportionate amounts of time on paperwork instead of patient care, which diminishes their job satisfaction and reduces the quality of care they can provide to patients.
The burden of these administrative tasks not only affects individual providers but also the overall healthcare system. With more time spent on completing paperwork, there is less time for direct patient interaction, leading to rushed appointments and potential oversights in care. Burnout among providers also contributes to higher turnover rates, further exacerbating the shortage of primary care providers. Effective strategies to streamline administrative processes and provide better support for care teams are crucial for alleviating workloads and enhancing both provider well-being and patient care quality.
Reducing Administrative Burdens
To address these issues, the HPC recommends that insurers overhaul program requirements and healthcare organizations enhance wages for care team staff to reduce turnover and provide better support for both patients and clinicians. By streamlining administrative processes and ensuring care teams are adequately supported, primary care providers can focus more on patient care rather than paperwork.
Implementing these recommendations would involve a systemic overhaul of current administrative practices, prioritizing ease of use and efficiency. For example, simplifying billing and coding processes and reducing the need for prior authorizations could significantly cut down on the time providers spend on non-clinical tasks. Moreover, increasing wages for supporting staff can help reduce turnover, ensuring that experienced and knowledgeable staff members are available to assist providers. These measures can contribute to a more efficient healthcare system where the primary focus remains on delivering high-quality care to patients.
Emergency Room Utilization
Patients Resorting to Emergency Rooms
A troubling trend in Massachusetts is the high volume of patients turning to emergency rooms because they cannot access primary care clinicians in a timely manner. This reliance on emergency rooms is not only costly but also inefficient, as these facilities are not designed for routine preventive care. The lack of access to primary care results in delayed diagnoses and treatments, leading to more severe health issues that could have been prevented with timely primary care.
The overutilization of emergency rooms for non-emergency medical needs places additional strain on an already overburdened healthcare system. It leads to longer wait times for actual emergencies and increases healthcare costs significantly. Furthermore, emergency rooms are not equipped to provide ongoing care management, which is essential for chronic condition management and preventive care. This gap in care continuity can result in poorer health outcomes for patients who rely on emergency services as their primary source of medical care.
Policy Recommendations to Address ER Utilization
The HPC has outlined various recommendations for lawmakers, healthcare organizations, and insurers to address the overreliance on emergency rooms for primary care. These include increasing the availability of primary care services, improving reimbursement rates, and reducing administrative burdens. By implementing these recommendations, it is possible to reduce the need for emergency room visits and ensure patients receive the care they need when they need it, leading to better health outcomes and lower overall healthcare costs.
Increasing the availability of primary care services involves not only attracting more providers to the field but also expanding service hours and locations to meet patient needs better. Improving reimbursement rates for primary care can make it a more viable career option for new graduates, helping to address the provider shortage. Reducing administrative burdens can free up more time for providers to see patients, improving access to care. Implementing these measures in tandem can create a more efficient and effective healthcare system, ultimately reducing the reliance on emergency rooms for non-urgent care.
Growing the Talent Pipeline
Expanding Medicaid Funding for Graduate Medical Education
There is a pressing need to grow the talent pipeline for primary care. In response, the HPC calls for the expansion of Medicaid funding for graduate medical education, including residencies, which Massachusetts discontinued in 2010. By reinstating this funding, the state can attract more medical graduates to primary care, thereby addressing the provider shortage and ensuring a steady influx of new practitioners into the field.
Expanding funding for graduate medical education is a crucial step towards addressing the state’s primary care shortage. Residencies offer essential training and experience for medical graduates, preparing them to enter the workforce as competent and confident providers. Reinstating Medicaid funding means more residency positions can be created, particularly in underrepresented areas such as primary care. This investment not only benefits individual graduates but also strengthens the overall healthcare system, ensuring that Massachusetts can meet the growing demand for primary care services.
Investments in Loan Repayment Programs
In addition to expanding Medicaid funding, investments in loan repayment programs for nurse practitioners and physician assistants are recommended. These programs provide financial incentives for new graduates to enter primary care, helping to alleviate the provider shortage. Adjustments to supervisory requirements for physician assistants to provide care independently are also suggested, enabling them to practice more autonomously and increase their capacity to serve patients.
Loan repayment programs are a powerful tool for attracting new graduates to the primary care field. By offering financial relief for student loans, these programs make primary care a more financially viable career option. Additionally, adjustments to supervisory requirements for physician assistants mean they can take on more responsibility and provide care directly to patients without extensive oversight. These changes can effectively expand the patient care capacity of the existing workforce, ensuring that more residents have access to the primary care services they need.
Expanding Investments in Primary Care
Shifting Payment Models
Increasing financial support for primary care is crucial for addressing the current crisis. The HPC recommends shifting payment models and rebalancing overall medical spending to increase investment in primary care. Specifically, insurers should adopt capitated payment models for primary care, wherein providers receive predictable and upfront payments. This model can provide financial stability for primary care practices and encourage more providers to enter the field, ultimately strengthening the primary care workforce.
Capitated payment models offer a significant advantage by providing predictable revenue streams for primary care practices. This financial stability allows practices to better manage their resources, invest in necessary infrastructure, and focus on delivering high-quality care without the constant pressure of fee-for-service billing. Additionally, shifting payment models to prioritize primary care spending can help balance the overall medical spending, making primary care a more attractive and sustainable career choice for new graduates. This shift is essential for ensuring a robust primary care workforce capable of meeting the growing healthcare needs of the state.
Supporting Independent Practices and Community Health Centers
Supporting independent primary care practices and community health centers is also essential. These practices often serve underserved populations and provide critical access to care. By increasing financial support and reducing administrative burdens, these practices can continue to provide high-quality care to their communities and play a pivotal role in the overall healthcare system.
Independent practices and community health centers are vital for ensuring that all residents, regardless of socioeconomic status, have access to primary care services. However, these practices face unique financial and administrative challenges that can hinder their ability to operate effectively. Providing targeted financial support and reducing administrative burdens can help these practices thrive and continue to serve their communities. Ensuring their sustainability is crucial for maintaining diverse and accessible healthcare options across the state, particularly in underserved areas where larger healthcare systems may not be present.
Task Force and Legislative Action
Creation of a Primary Care Task Force
A significant step towards addressing the primary care crisis in Massachusetts is the creation of a new primary care task force, born from the recent hospital and market oversight law. This task force is tasked with refining and expanding the HPC’s recommendations, focusing on the critical issues of provider shortage, financial disparities, and administrative burdens. This collaborative effort aims to develop comprehensive and actionable solutions that will strengthen the primary care system across the state.
The establishment of the primary care task force marks a proactive approach to tackling the challenges facing the primary care workforce. By bringing together stakeholders from various sectors, including policymakers, healthcare organizations, and insurers, the task force can ensure that proposed solutions are holistic and consider the perspectives of all parties involved. This collaborative effort is essential for addressing the multifaceted nature of the primary care crisis and ensuring that proposed solutions are both effective and sustainable in the long term.
Legislative Support and Budgetary Considerations
Legislative support is pivotal for the success of the HPC’s recommendations. With Governor Maura Healey and Senate President Karen Spilka showing interest, concrete plans for state investment are still developing. The fiscal 2026 budget planning includes a 2.2% tax revenue growth estimate, which must account for the new initiatives proposed by the HPC. Adequate budgetary support will be crucial for implementing the recommended strategies and ensuring that the primary care system receives the necessary resources to thrive.
Securing the necessary budgetary allocations will require strong advocacy and collaboration between state leaders and healthcare stakeholders. The anticipated tax revenue growth can provide a crucial funding source for the various initiatives needed to bolster the primary care workforce and improve access to care. Legislative action will also be necessary to enact the policy changes proposed by the HPC, including adjustments to reimbursement rates, funding for graduate medical education, and support for independent practices. Ensuring sustained legislative support and adequate funding will be key to the successful implementation of these strategies and the long-term stability of the primary care system in Massachusetts.
Main Findings
The main findings from the analysis of the HPC’s recommendations and related data reveal several pressing needs and action areas. First, there is an urgent requirement to address the provider shortage in primary care to ensure all residents have access to basic health services. Second, financial incentives are currently skewed towards specialty care, necessitating a rebalancing of reimbursement rates and payment models to make primary care more attractive to new graduates. Third, the administrative burdens on providers must be alleviated to reduce burnout and improve job satisfaction, enhancing the overall care quality. Lastly, investments in training and financial support for new providers, coupled with legislative action, are essential for implementing these recommendations effectively.
The success of these initiatives will depend on coordinated efforts from all stakeholders involved. Addressing the provider shortage requires both immediate and long-term strategies to attract and retain primary care providers. Financial incentives must be realigned to make primary care a more viable and appealing career path for medical graduates. Reducing administrative burdens will require systemic changes to streamline processes and support care teams. Furthermore, investments in training programs, loan repayment initiatives, and legislative support will be crucial for sustaining the primary care workforce and ensuring that the healthcare system in Massachusetts can meet the needs of its residents.
Moving Forward with Proactive Steps
The primary care workforce in Massachusetts is under immense pressure, leaving residents struggling to access essential preventive care services. This escalating crisis results in patients frequently being unable to receive timely and critical healthcare necessary for their overall well-being. To address this worsening situation, the Massachusetts Health Policy Commission (HPC) has put forward a series of innovative recommendations aimed at resolving the issue and enhancing healthcare accessibility across the state.
This analysis delves into the prevalent themes, significant points, major trends, and shared views surrounding the primary care shortage. It also highlights the pragmatic proposals suggested by the HPC. The recommendations are designed to alleviate the current stress on the healthcare system, ensuring that residents receive the preventive care they need without unnecessary delays. The effort includes exploring ways to improve workforce retention, expanding training programs for primary care providers, and implementing policy changes that support sustainable primary care practices.