Imagine a life where pain persists relentlessly for months or even years, with no apparent injury or obvious remedy in sight, leaving sufferers feeling isolated and misunderstood. For approximately one in five Canadians, chronic pain is not just an occasional discomfort but a daily battle, often dismissed as a psychological quirk or exaggerated complaint. This “invisible” condition has long evaded effective treatment due to a lack of understanding about its true nature. However, a pioneering research effort at St. Joseph’s Health Care London in Canada, under the guidance of Dr. Siobhan Schabrun, is poised to change this narrative. By focusing on the brain’s critical role in perpetuating pain long after physical healing, this initiative seeks to transform how chronic pain is diagnosed and managed. Supported by the Workplace Safety and Insurance Board (WSIB), the project offers a glimmer of hope for millions, promising not only better care but also a shift in societal perception of this pervasive issue.
Unraveling the Brain’s Role in Pain
Chronic pain has historically been misunderstood, often attributed to lingering physical damage or mental health struggles rather than a distinct medical issue. Research led by Dr. Schabrun challenges these outdated assumptions by demonstrating that the brain and spinal cord can undergo a process of rewiring after an initial injury. Even when tissues have fully healed, these neural changes can sustain pain signals, creating a cycle of discomfort that defies traditional explanations. This neurological perspective redefines chronic pain as a condition rooted in the central nervous system, not merely a prolonged symptom of injury. Such a shift in understanding is vital for developing treatments that address the true source of suffering, moving beyond surface-level interventions that often fall short. It also lays the groundwork for reducing the stigma that has long plagued those who live with this condition, validating their experiences with solid scientific evidence.
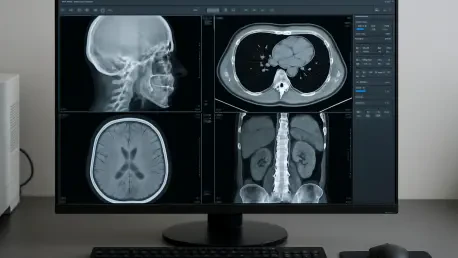
The implications of viewing chronic pain through a neurological lens are profound, especially for how medical professionals approach diagnosis and care. Instead of focusing solely on the site of an original injury, attention must turn to the brain’s altered pathways that keep pain alive. This research underscores the need for innovative tools to map these changes, providing a clearer picture of why some individuals transition from acute to chronic pain while others do not. By identifying specific patterns in brain activity, scientists can better predict who is at risk and tailor interventions accordingly. This approach marks a departure from the one-size-fits-all strategies that have dominated pain management for decades, offering a more personalized and potentially effective framework. As this field evolves, it could fundamentally alter the trajectory for countless patients, turning a once-invisible struggle into a treatable condition with a defined biological basis.
Pioneering New Treatment Pathways
Traditional methods of treating chronic pain often center on the physical location of an injury, such as prescribing painkillers or recommending physical therapy, but these frequently fail to provide lasting relief. The team at St. Joseph’s Health Care London is taking a radically different tack by leveraging advanced brain imaging to detect early markers that signal a likelihood of chronic pain development following an acute injury. Identifying these indicators at the outset opens the door to preemptive measures that could halt the progression of pain before it becomes entrenched. Techniques like non-invasive brain stimulation are being explored to disrupt harmful neural patterns, offering a potential lifeline to those at risk. This brain-centric strategy represents a significant leap forward, prioritizing the underlying mechanisms over mere symptom management, and could redefine standards of care for millions.
Beyond diagnostic innovation, the focus on brain-based interventions highlights a critical gap in current medical practice—namely, the oversight of neurological factors in pain persistence. While conventional treatments might alleviate discomfort temporarily, they rarely address the rewired pathways in the brain that sustain chronic states. The research initiative aims to bridge this gap by testing methods that directly influence neural activity, potentially resetting the brain’s response to pain. If successful, such approaches could reduce reliance on medications with significant side effects, like opioids, and instead offer sustainable solutions rooted in neuroscience. This shift not only promises better outcomes for individual patients but also has broader implications for healthcare systems burdened by the long-term costs of ineffective pain management. As these methods gain traction, they could set a new benchmark for addressing one of medicine’s most stubborn challenges.
Enhancing Workplace Safety and Support
Workplace injuries, particularly in high-risk industries like construction or manufacturing, often serve as the starting point for chronic pain, creating a pressing need for better management strategies. The research supported by the WSIB provides actionable insights for health and safety leaders tasked with protecting workers. By recognizing chronic pain as a neurological condition rather than a lingering physical ailment, employers can adopt early intervention protocols based on brain assessments to identify at-risk individuals. Such measures could prevent the transition to long-term disability, preserving both employee health and productivity. Moreover, fostering a workplace culture that acknowledges chronic pain as a legitimate issue helps dismantle stigma, encouraging workers to report symptoms without fear of skepticism or judgment, ultimately leading to more effective support systems.
The economic and social benefits of integrating this research into workplace policies cannot be overstated, as chronic pain often results in extended absences and reduced quality of life for affected workers. Health and safety professionals now have an opportunity to implement science-backed approaches, such as tailored rehabilitation programs informed by neurological data, to mitigate these outcomes. Collaboration with medical experts to incorporate brain-focused screenings after injuries could become a standard practice, ensuring that potential chronic pain cases are caught early. This proactive stance not only aids individual recovery but also reduces the financial strain on businesses and insurance systems caused by prolonged disability claims. As industries begin to adopt these findings, the ripple effect could transform occupational health standards, creating environments where worker well-being is prioritized through cutting-edge understanding of pain’s true nature.
Bridging Gaps in Medical Understanding
Chronic pain’s complexity has long been underestimated due to the fragmented way in which related fields like musculoskeletal health, mental health, and pain studies have been approached. Historically, these disciplines operated in isolation, hindering a comprehensive grasp of how pain persists and impacts lives. The initiative at St. Joseph’s Health Care London seeks to unify these areas, recognizing that physical, neurological, and emotional factors are deeply intertwined in chronic pain experiences. This interdisciplinary effort is paving the way for treatment models that address the whole person rather than isolated symptoms, offering a more robust framework for care. By integrating insights from diverse medical perspectives, the research promises to deliver strategies that are both innovative and inclusive, better equipped to tackle the multifaceted nature of this condition.
This push toward integration also reflects a broader trend in medical science to move beyond siloed research and embrace collaborative solutions for complex health challenges. Understanding chronic pain as a condition that spans multiple domains allows for the development of interventions that are more effective because they account for overlapping influences, such as how stress or trauma might amplify pain signals in the brain. Such a holistic view could reshape clinical practices, encouraging healthcare providers to consider a wider range of factors when designing treatment plans. Additionally, this approach has the potential to influence policy in occupational health, where integrated care models could support workers more comprehensively after injuries. As this paradigm gains momentum, it sets a precedent for addressing other intricate health issues, demonstrating the power of unified scientific inquiry in improving patient outcomes across various contexts.
Shifting Societal Perceptions of Pain
Despite its prevalence, chronic pain often remains a hidden burden, misunderstood by society and even by some within the medical community, leaving many to suffer in silence. A central aim of the ongoing research, as highlighted by Dr. Aaron Thompson of WSIB, is to combat this stigma by firmly establishing chronic pain as a legitimate diagnosis grounded in neurological changes. This validation is crucial for altering public perception, ensuring that those affected are no longer dismissed as exaggerating their condition or lacking resilience. Raising awareness about the biological basis of chronic pain can foster empathy and encourage open conversations, breaking down barriers that prevent sufferers from seeking help. Such a cultural shift is essential for creating a society where this condition is met with understanding rather than skepticism.
Building on this foundation, the effort to destigmatize chronic pain extends beyond individual recognition to systemic change in how healthcare and workplace environments respond. Educating the public and professionals alike about the brain’s role in sustaining pain can lead to more compassionate policies and practices, ensuring that patients receive timely and appropriate care. This research serves as a catalyst for dialogue, prompting discussions that challenge long-held misconceptions and replace them with evidence-based perspectives. By highlighting the tangible, scientific underpinnings of chronic pain, it becomes possible to advocate for resources and support systems that address the real needs of those impacted. Over time, these efforts could redefine societal attitudes, transforming chronic pain from an invisible struggle into a widely acknowledged health priority that demands attention and action from all sectors.